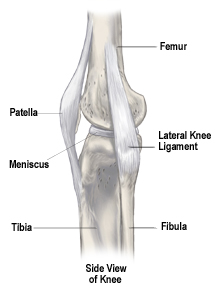
 The knee is a hinge joint consisting
of three bones. The upper part of
the hinge is at the end of the upper
leg bone (femur), and the lower part
of the hinge is at the top of the
lower leg bone (tibia). When the
knee is bent, the end of the femur
rolls and slides on top of the
tibia. A third bone, the kneecap
(patella), glides over the front and
end of the femur.
The knee is a hinge joint consisting
of three bones. The upper part of
the hinge is at the end of the upper
leg bone (femur), and the lower part
of the hinge is at the top of the
lower leg bone (tibia). When the
knee is bent, the end of the femur
rolls and slides on top of the
tibia. A third bone, the kneecap
(patella), glides over the front and
end of the femur.
In a
healthy knee joint, the surfaces of
these bones are very smooth and
covered with a tough protective
tissue called cartilage. Arthritis
causes damage to the bone surfaces
and cartilage where the three bones
meet and rub together. These damaged
surfaces can eventually become
painful.
There are
several ways to treat the pain
caused by arthritis. One way is
total knee replacement surgery. The
decision to have total knee
replacement surgery should be made
very carefully after consulting your
doctor and learning as much as you
can about the knee joint, arthritis,
and the surgery.
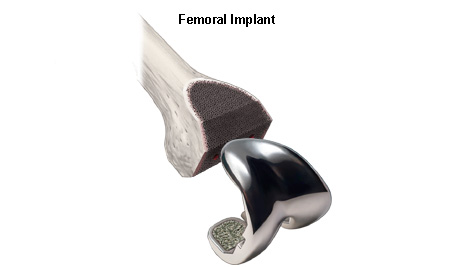
In total
knee replacement surgery, the bone
surfaces and cartilage that have
been damaged by arthritis are
removed and replaced with artificial
surfaces made of metal and a plastic
material. We call these artificial
surfaces “implants,” or
“prostheses.”

What to
Bring to the Hospital
Below is a
list of things you may want to bring
with you to the hospital in
preparation for your surgery. Talk
with your physician, as he/she may
have additional information about
preparing for your hospital stay.
- Your
personal belongings should be
left in the car until after
surgery. Tell your family that
your room will be assigned when
you are in surgery or in
recovery, at which point they
can bring your personal items to
your room.
-
Personal grooming items that you
may want to pack include a
toothbrush, toothpaste,
hairbrush, eyeglasses/contacts,
comb, deodorant, shaving
cream/electric razor, shampoo,
lotion, undergarments, and a
robe.
- Bring
slippers or flat rubber-soled
shoes for walking in the
hallways.
- Bring
loose fitting clothing for your
trip home.
- Bring
any medications you are
currently taking. You should
also write down your medication
information to be given to the
hospital staff. Be sure to
include the name, strength, and
how often you take the
medications. Please communicate
any allergies you might have to
your doctors and the nursing
staff.
- If you
use a breathing exerciser (IBE),
be sure to bring it with you
from home, as you will probably
need this right after surgery.
- Leave
jewelry, credit cards, car and
house keys, checkbooks, and
items of personal value at home.
Bring only enough pocket money
for items such as newspapers,
magazines, etc.
During
Surgery
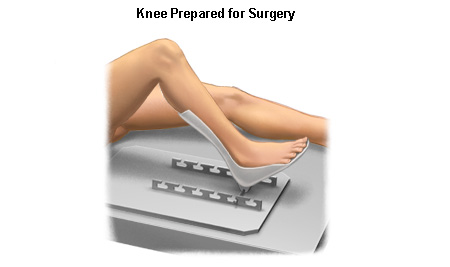
The patient
is first taken into the operating
room and given anesthesia. After the
anesthesia has taken effect, the
skin around the knee is thoroughly
scrubbed with an antiseptic liquid.
The knee is flexed about 90 degrees
and the lower portion of the leg,
including the foot, is placed in a
special device to securely hold it
in place during the surgery. Usually
a tourniquet is then applied to the
upper portion of the leg to help
slow the flow of blood during the
surgery. An incision of appropriate
size is then made.
Removing
the Damaged Bone Surfaces
The damaged
bone surfaces and cartilage are then
removed by the surgeon. Precision
instruments and guides are used to
help make sure the cuts are made at
the correct angles so the bones will
align properly after the new
surfaces (implants) are attached.
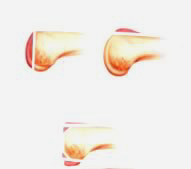 Small amounts of the bone surface
are removed from the front, end, and
back of the femur. This shapes the
bone so the implants will fit
properly.The amount of bone that is
removed depends on the amount of
bone that has been damaged by the
arthritis.
Small amounts of the bone surface
are removed from the front, end, and
back of the femur. This shapes the
bone so the implants will fit
properly.The amount of bone that is
removed depends on the amount of
bone that has been damaged by the
arthritis.
A small
portion of the top surface of the
tibia is also removed, making the
end of the bone flat.
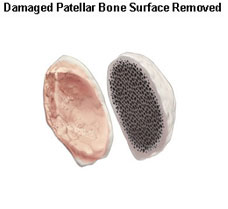
The back
surface of the patella (kneecap) is
also removed.

Attaching
the Implants
An implant
is attached to each of the three
bones. These implants are designed
so that the knee joint will move in
a way that is very similar to the
way the joint moved when it was
healthy. The implants are attached
using a special kind of cement for
bones.
The implant
that fits over the end of the femur
is made of metal. Its surface is
rounded and very smooth, covering
the front and back of the bone as
well as the end.
The implant
that fits over the top of the tibia
usually consists of two parts. A
metal baseplate fits over the part
of the bone that was cut flat. A
durable plastic articular surface is
then attached to the baseplate to
serve as a spacer between the
baseplate and the metal implant that
covers the end of the femur.

The implant
that covers the back of the patella
is also made of a durable plastic.

Artificial
knee implants come in many designs.
Some designs may have pegs,
requiring small holes to be drilled
into the bone after the damaged
surfaces have been removed. Others
may have central stems. In addition,
some designs may allow screws to be
used on the lower implant to provide
added attachment security. The
surgeon will choose the implant
design that best meets the patient’s
needs.

Closing
the Wound
If necessary,
the surgeon may adjust the ligaments
that surround the knee to achieve
the best possible knee function.
When all of
the implants are in place and the
ligaments are properly adjusted, the
surgeon sews the layers of tissue
back into their proper position. A
plastic tube may be inserted into
the wound to allow liquids to drain
from the site during the first few
hours after surgery. The edges of
the skin are then sewn together, and
the knee is wrapped in a sterile
bandage. The patient is then taken
to the recovery room.